Chief Medical Officer reporting the events of Captain Brennan’s birth
Captain Brennan’s birth begins Tuesday May 24th. I was at my desk working and at about 3:15 pm I felt a painful contraction. A few minutes later I felt another one. The next one came at 3:24 pm and so I began timing them as I tried the usual, drink water, empty bladder, change positions. But I knew these contractions were different than the painless Braxton Hicks ones experienced previously and the usual techniques did not alter them so I called Mayo at 3:50 pm. As expected I was told to come in immediately given my history. I got in the car at about 4pm, calling the Admiral on the way to the hospital. I parked and made it to OB triage by 4:15. The admiral joined me soon after.
I was hooked up to two monitors. One that measured the frequency and severity of the contractions and the other that monitored the captain’s heart rate. We waited about hour for the resident to come in and check for dilation. In the meantime my contractions were about 2-3 mins apart and gaining in severity. The resident checked and I was about 75% effaced and 3 cm dilated and my cervical length was less than 1 cm (not good). I was sent to labor and delivery to see what my body would do.
In labor in deliver I was hooked up to the monitors and an IV and given fluids (dehydration can cause contractions), I went the bathroom (a full bladder can cause contractions) and given antibiotics (a UTI or other infection can cause contractions). Finally, I was given the first round of a series of steroid shots for Captain’s lungs at about 7pm. The next shot was due at 7pm the next day and the longer the Captain stayed in me while these shots worked the less likely his lungs would be underdeveloped. I was also given medicine (nifedipine) to try and stop my contractions.
Contractions seemed to ease up for a couple hours. During this time the NNP (Neonatal Nurse Practitioner) came in to give a consult. She was very nice and explained that 32 weeks was very different than 26 weeks and that most of these babies don’t even have to go the NICU at St. Mary’s but stay at the Level II, Intermediate Special Care Nursery. The Admiral and I were hopeful. Then the Admiral ran home to get some supplies. He didn’t want to leave me, but we’d been down this road before.
By the time he made it back the contractions were stronger than ever and very painful. I asked for pain relief and first received fentanyl, which made me dizzy and very hot. Then my uterus wouldn’t relax between contractions. This caused the Captain’s heartbeat to slow down. A crew of doctors and nurses came in and there was some concern about the Captain at this point. (Note: a previous post by the Admiral stated that the Captain’s heartbeat stopped, this was creative license. The Captain’s heart did not stop, it did slow down to a worrisome point, but never stopped). I was given medicine to help my uterus relax between contractions, but that medicine caused my heart rate to skyrocket. There were some tense moments where both mom and baby were not doing well, but after a little while they both rebounded. I was then checked again at about 11 pm and was fully effaced but still only 3 cm dilated.
I got an epidural after this incident hoping to make it with the Captain still inside until that next steroid shot at 7pm. The epidural allowed us to get some rest. We watched the Cubs vs. Cardinals on the Admiral’s tablet and both eventually fell asleep. At 2am the doctors came in and checked me again. I was now 5 cm dilated and fully effaced. I got more medicine for the contractions, which gave me awful nausea and I proceeded to throw up and dry heave for a little while. I was able to fall back asleep for another hour or so.
At 330am I was awoken by my nurse pulling back the curtain. She said the doctors wanted to check me again. She had seen something on the monitors while I was sleeping. Sure enough the doctors checked and I was complete (100% effaced and fully dilated to 10 cm). The doctor said he could feel my membranes but that my water had not broken yet so it was time to deliver the baby. I was very concerned that we didn’t make it the full 24 hours to the next steroid shot. Wheeled down to the OR (where all preemies are born) I remembered the same trip with Finn. I can’t even begin to describe how terrifying and surreal this whole experience was. Determined to do things differently the Admiral and I decided that no matter what happened he was to stay with the Captain so he wasn’t alone.
My water was broken and the doctors commented that there was more blood than expected. It’s possible I had another Placental Abruption. I pushed and pushed and as the Admiral held my hand Captain Brennan was born crying, a vigorous male, at 4:11 am at 32 weeks and 6 days gestational age.
Admiral and the Captain were taken to the nearby room where preemies are taken and evaluated. While I was cleaned up and delivered the placenta the Admiral stayed with the Captain the whole time. I was wheeled over to see the Captain on the way back to her room. He was pink and squirmy but was on a Cpap machine to help him struggle less to breathe.
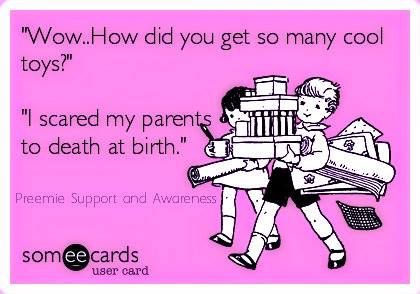
An hour later mom was told by the Rns that the captain was struggling to breathe too much, he need to be intubeated, and given surfactant, which meant a trip to the St. Mary’s Nicu. To say I was devastated by this news is a monumental understatement. It felt like Finnegan all over again. I thought “I am going to lose this baby too” and “when I lose Brennan I won’t be able to go on.”
The nurses and the doctors all became concerned with my sudden change in affect at this news and patiently explained how different 32 (almost 33) weeks was than a 26 weeker like. It helped a little but really it felt like it was all happening again and I’ve been down this path and I know how it ends. These were the most difficult hours for me, but I was determined to do things differently this time.
The nurses said I could transfer to St. Mary’s to be nearer the Captain for post partum. I had been transferred with Finn and it was a disaster. There were poor logistics, confused nurses, callous doctors and whole communication screw up regarding my Rhogm shot. This communication screw up caused me to lose precious moments of Finn’s life and I wouldn’t do it again.
So I said no to the transfer and requested discharge as soon as possible. I had pretty much decided that if they wouldn’t discharge me I was just going to leave as soon as I could walk. The team of doctors came in and talked to with me about what I wanted to do. But I wasn’t taking no for an answer.
The Admiral didn’t want me driving so about 6 hours after delivering a baby an escort wheeled me down to the street and the Admiral picked me up and I was discharged. When we got to St. Mary’s the Admiral had me wait in a wheel chair while he parked the car and then wheeled me up to the NICU where I got be with the Captain all afternoon.